Did you know that early detection can increase the chances of successful breast cancer treatment by up to 98%? Breast cancer is one of the most common forms of cancer, affecting millions of women worldwide. Taking proactive steps towards early detection can save lives and improve outcomes. In this comprehensive guide, we will provide you with essential information on how to check for breast cancer and the steps you can take for early detection.
Key Takeaways:
- Early detection greatly improves the chances of successful breast cancer treatment.
- Breast cancer is a common form of cancer that affects millions of women.
- Knowing how to check for breast cancer is essential for early detection.
- Regular self-exams, clinical breast exams, and mammograms are important screening methods.
- Understanding breast cancer risk factors and adopting a healthy lifestyle can help in prevention.
Understanding Breast Cancer: Signs and Symptoms
Before learning how to check for breast cancer, it’s important to be aware of the signs and symptoms. Recognizing these symptoms can prompt further action and medical evaluation. Here are some common signs of breast cancer:
- Breast lumps: These can be felt as a hard mass or thickening in the breast or armpit area.
- Changes in breast size or shape: Any unexplained changes in the size or shape of the breast should be monitored closely.
- Nipple discharge: Discharge other than breast milk, especially if it is bloody or occurs spontaneously, should be evaluated by a healthcare professional.
- Skin changes: Dimpling, puckering, redness, or scaliness of the breast skin can be potential symptoms of breast cancer.
If you experience any of these signs, it’s important to consult your healthcare provider for further evaluation. While these symptoms can be indicative of breast cancer, they can also have other benign causes. Your healthcare provider may recommend additional tests or imaging to determine the cause of your symptoms.
“Early detection of breast cancer greatly improves treatment outcomes and survival rates.”
Being aware of the signs and symptoms of breast cancer empowers individuals to take control of their breast health and seek timely medical attention when needed. Remember, early detection plays a vital role in successful treatment and outcomes.
Risk Factors for Breast Cancer
Certain factors can increase the risk of developing breast cancer. Understanding these risk factors is crucial in assessing your personal risk and taking appropriate preventive measures.
Age
Age is a significant risk factor for breast cancer. The risk increases as you get older, with most cases occurring in women over the age of 50.
Family History
A family history of breast cancer can increase your risk, especially if you have a first-degree relative (such as a parent or sibling) who has been diagnosed with the disease. Genetic mutations, such as BRCA1 and BRCA2, can also contribute to a higher risk.
Genetics
Genetic factors play a role in breast cancer risk. Mutations in specific genes, such as BRCA1 and BRCA2, can increase the likelihood of developing the disease. Genetic counseling and testing may be recommended for individuals with a strong family history of breast cancer.
Hormonal Factors
Hormonal factors, such as early menstruation (before age 12) and late menopause (after age 55), can increase the risk of breast cancer. Additionally, women who have undergone hormone replacement therapy (HRT) for an extended period may have a higher risk.
Lifestyle Choices
Lifestyle choices can also influence breast cancer risk. Factors such as obesity, excessive alcohol consumption, and a sedentary lifestyle can increase the likelihood of developing the disease. On the other hand, maintaining a healthy weight, engaging in regular physical activity, and limiting alcohol intake can help reduce the risk.
“Understanding the risk factors associated with breast cancer is essential in taking proactive steps towards prevention and early detection.”
In summary, being aware of the risk factors for breast cancer can empower you to make informed decisions about your health. By understanding the role of age, family history, genetics, hormonal factors, and lifestyle choices, you can take proactive steps to reduce your risk and prioritize regular screenings. Stay vigilant and consult with your healthcare provider for personalized guidance and support.
Breast Cancer Self-Exam: Step-by-Step Guide
Performing regular breast self-exams is a crucial part of maintaining breast health and detecting any possible abnormalities. By familiarizing yourself with the normal look and feel of your breasts, you can quickly identify any changes or potential concerns. Follow this step-by-step guide to conduct a thorough breast self-exam:
- Begin by visually inspecting your breasts. Stand in front of a mirror with your arms at your sides and carefully observe your breasts. Look for any changes in size, shape, or skin texture. Check for any visible lumps or dimpling.
- Next, raise your arms overhead and look for the same changes as in the previous step.
- While still in front of the mirror, examine your nipples. Look for any signs of discharge, such as blood or fluid other than breast milk.
- Move on to the palpation stage of the exam. Lie down on a comfortable surface and use the pads of your fingers to gently press in a circular motion around your breast. Start from the outer edges and gradually move toward the center. Ensure you cover the entire breast, including the armpit area.
- Pay attention to the texture and consistency of your breast tissue. While performing the palpation, be on the lookout for any lumps or thickening. Note any changes in tenderness or pain.
- Repeat steps 4 and 5 while standing or sitting. Use the same circular motion to examine your breasts while standing or sitting. This allows you to feel for any differences in texture or lumps when the breast tissue is in a different position.
If you notice any changes, such as the presence of a breast lump, skin dimpling, nipple inversion, or any other abnormalities, it is essential to consult with your healthcare provider promptly. Remember that most breast lumps are not cancerous, but it’s crucial to get any changes evaluated by a medical professional.
Regular breast self-exams, along with clinical breast exams and mammograms, play a significant role in early detection and improving outcomes for breast cancer. By taking charge of your breast health, you empower yourself with knowledge and take proactive steps in your well-being.
| Benefits of Breast Self-Exams: | Tips for Conducting Breast Self-Exams: |
|---|---|
| 1. Early detection of breast abnormalities | 1. Perform the exam once a month, preferably a week after your period ends |
| 2. Improved familiarity with your breasts’ normal look and feel | 2. Use the pads of your fingers and apply gentle pressure during palpation |
| 3. Increased peace of mind and confidence in your breast health | 3. If you have undergone a mastectomy or breast reconstruction, adjust the self-exam process accordingly |
| 4. Empowerment and proactive approach to your well-being | 4. Remember that not all abnormalities are cancerous, but they should be evaluated by a healthcare professional |
Clinical Breast Exams and Mammograms
Clinical breast exams and mammograms are vital components of breast cancer screening. Regular screenings increase the chances of early detection, leading to improved outcomes. Understanding the procedures involved, when to start getting them, and the recommended frequency is essential for every individual’s breast health.
What is a Clinical Breast Exam?
A clinical breast exam, also known as a physical breast exam, is conducted by a healthcare professional. During the exam, the healthcare provider carefully examines your breasts, looking for any abnormalities, changes, or signs of breast cancer. This exam is an opportunity to discuss any concerns, symptoms, or family history related to breast health.
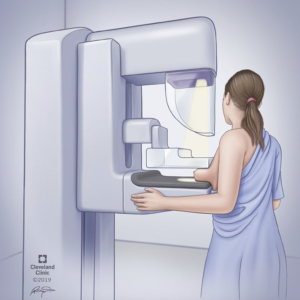
What is a Mammogram?
A mammogram is an X-ray of the breasts that can detect early signs of breast cancer, such as lumps or calcifications. It is performed using a specialized machine that compresses the breasts between two plates, allowing for a clear and detailed image. Mammograms are essential in detecting breast cancer at its earliest stages, even before any noticeable symptoms appear.
When and How Often to Get Screened?
The recommended age to start clinical breast exams and mammograms may vary depending on individual risk factors and guidelines. The American Cancer Society suggests that women should have yearly mammograms starting at age 40. However, it’s crucial to discuss with your healthcare provider to assess your personal risk and determine the best screening plan for you.
The Benefits of Early Detection
Early detection through clinical breast exams and mammograms significantly increases the chances of successful treatment and survival. Detecting breast cancer in its early stages allows for more treatment options and better outcomes. Regular screenings empower individuals to take proactive control of their breast health.
Comparison of Clinical Breast Exams and Mammograms
| Screening Method | Advantages | Limitations |
|---|---|---|
| Clinical Breast Exam | – Performed by healthcare professionals – Allows for discussion of concerns and symptoms – Detects abnormalities that may not be visible on mammograms |
– Dependent on the skill and experience of the examiner – May miss small tumors or abnormalities – Additional imaging or biopsy may be required for further evaluation |
| Mammogram | – Captures detailed images of breast tissue – Detects small tumors or calcifications – Widely available and established screening method |
– May result in false positives or false negatives – Radiation exposure (minimal) – Limited effectiveness in women with dense breast tissue |
It’s important to note that clinical breast exams and mammograms are complementary screening methods. Regular screenings, along with self-exams and awareness of any changes in your breasts, enhance the proactive approach to breast health. Remember, early detection is key to better treatment options and improved outcomes.
Understanding Breast Biopsies
When an abnormality is detected during breast cancer screening or self-exams, further evaluation through a breast biopsy may be recommended. A breast lump, for example, often warrants a biopsy to determine if it is benign or cancerous. Understanding the different types of breast biopsies can help alleviate any concerns or fears.
Types of Breast Biopsies
There are three common types of breast biopsies:
- Fine-Needle Aspiration (FNA) Biopsy: This minimally invasive procedure involves the use of a thin needle to extract a small sample of cells or fluid from the breast lump for analysis. FNA biopsies are often used to evaluate the nature of a cyst or a solid mass.
- Core Needle Biopsy: In this procedure, a larger needle is used to extract several tissue samples from the breast lump. These samples are then sent to a laboratory for microscopic examination. Core needle biopsies are effective in diagnosing both benign and malignant breast conditions.
- Surgical Biopsy: If the previous biopsies do not yield conclusive results or if the detected abnormality requires complete removal, a surgical biopsy may be performed. This procedure involves removing the entire lump or a significant portion of it for further examination.
It’s important to note that the type of biopsy recommended depends on the specific characteristics of the breast lump and the diagnostic goals of the healthcare professional.
| Type of Biopsy | Procedure | Advantages | Disadvantages |
|---|---|---|---|
| Fine-Needle Aspiration (FNA) Biopsy | Thin needle insertion to extract cells or fluid from the lump. | – Minimally invasive – Quick results |
– Limited sample size – Possible need for additional procedures |
| Core Needle Biopsy | Larger needle insertion to extract tissue samples from the lump. | – More definitive diagnosis – Less invasive than surgical biopsy |
– Slight risk of bleeding or infection |
| Surgical Biopsy | Surgical removal of the lump or a significant portion of it. | – Complete removal and analysis – Accurate diagnosis of complex cases |
– Surgical risks – Longer recovery time |
It’s important to remember that a breast biopsy is a routine procedure and is generally well-tolerated. Your healthcare provider will discuss the most appropriate type of biopsy for your specific situation and provide guidance and support throughout the process.
Genetic Testing and Breast Cancer
Genetic testing plays a crucial role in determining an individual’s risk of developing breast cancer. By analyzing your genetic makeup, medical professionals can provide valuable insights into your susceptibility to the disease. Understanding the impact of genetics on breast cancer risk empowers individuals to make informed decisions about prevention and treatment.
BRCA Gene Mutations: One of the key genetic factors associated with breast cancer risk is mutations in the BRCA genes. These genes, BRCA1 and BRCA2, are responsible for repairing damaged DNA and suppressing the growth of abnormal cells. Mutations in these genes can significantly increase the likelihood of developing breast and ovarian cancer.
“Genetic testing can identify these BRCA gene mutations, enabling individuals to better understand their risk profiles and take appropriate preventive measures,” explains Dr. Laura Thompson, a renowned genetic counselor.
Genetic Counseling and Testing: To determine whether genetic testing is necessary, individuals with a family history of breast cancer or certain risk factors should consult with a genetic counselor. These healthcare professionals specialize in assessing personal and family medical histories to identify potential genetic risks. They provide guidance and support throughout the testing process.
Genetic testing is typically conducted through a simple blood or saliva test. The sample is sent to a laboratory, where it is analyzed for specific genetic markers associated with breast cancer. The results are then interpreted by genetic counselors or healthcare providers to assess the individual’s risk.
Benefits of Genetic Testing:
Genetic testing offers several benefits in relation to breast cancer:
- Identifying high-risk individuals: Testing helps identify individuals who have an elevated genetic risk for breast cancer, allowing for proactive monitoring, early detection, and timely intervention.
- Informed decision-making: Understanding your genetic risk empowers you to make informed decisions about preventive measures, such as increased surveillance, lifestyle modifications, or even prophylactic surgeries.
- Targeted treatment: In cases where breast cancer is diagnosed, genetic testing can influence treatment decisions by providing insights into potential treatment responses and guiding the selection of targeted therapies.
It is essential to approach genetic testing with a comprehensive understanding of its implications. Genetic counselors play a crucial role in guiding individuals through the testing process, interpreting results, and providing emotional support.
Genetic testing is not only beneficial for individuals but can also have broader implications for families. With knowledge of genetic risk factors, family members can make informed decisions about their own health and undergo appropriate testing if necessary.
By exploring the role of genetics in breast cancer risk and undergoing genetic testing, individuals can take proactive steps towards prevention, early detection, and personalized treatment strategies.
| Genetic Testing and Breast Cancer | Benefits |
|---|---|
| Identification of high-risk individuals | Allows for proactive monitoring and intervention |
| Informed decision-making | Empowers individuals to make personalized choices |
| Targeted treatment | Guides treatment decisions and improves outcomes |
Genetic testing provides valuable insights into breast cancer risk and helps individuals make informed decisions about their health. By understanding genetic factors and consulting with genetic counselors, individuals can take proactive measures to minimize their risk and lead healthier lives.
Promoting Breast Health: Lifestyle and Prevention
Adopting a healthy lifestyle is crucial in reducing the risk of breast cancer. By making conscious choices and incorporating preventive measures into your daily routine, you can prioritize your breast health. Let’s explore the key lifestyle factors that contribute to breast health and lower the risk of breast cancer.
Maintain a Healthy Weight
Maintaining a healthy weight is essential for overall health and plays a significant role in breast cancer prevention. Obesity has been linked to an increased risk of breast cancer, especially in postmenopausal women. Excess body fat produces hormones that can stimulate the growth of breast cancer cells. By maintaining a healthy weight through a balanced diet and regular exercise, you can reduce your risk of developing breast cancer.
Regular Exercise
Engaging in regular physical activity not only helps maintain a healthy weight but also provides numerous health benefits, including reducing the risk of breast cancer. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity each week. Incorporate activities such as brisk walking, cycling, swimming, or dancing into your routine. Regular exercise can also improve overall well-being and reduce stress levels.
Limit Alcohol Consumption
Limiting alcohol consumption is vital for breast health. Research has shown that excessive alcohol consumption is associated with an increased risk of breast cancer. If you choose to drink alcohol, it is recommended to moderate your intake. The American Cancer Society suggests limiting alcohol to one drink per day for women. Abstaining from alcohol is the best option for reducing your breast cancer risk.
Breastfeeding
For mothers, breastfeeding offers both health benefits for the baby and potential protection against breast cancer. Studies have shown that breastfeeding reduces the risk of breast cancer, particularly in women who breastfeed for a longer duration. Breastfeeding helps regulate hormone levels and reduces the number of menstrual cycles a woman experiences in her lifetime, which can lower the risk of breast cancer.
Regular Check-ups and Screenings
Regular check-ups and screenings are essential for early detection and maintaining breast health. Schedule regular visits with your healthcare provider for a comprehensive evaluation of your breast health. Follow recommended screening guidelines, such as clinical breast exams and mammograms, based on your age and risk factors. Early detection can significantly improve treatment outcomes. Remember to consult with healthcare professionals for personalized guidance and support.
“By adopting a healthy lifestyle and following recommended screening guidelines, you can take proactive steps towards promoting breast health and reducing the risk of breast cancer.”
– Dr. Sarah Thompson, Oncologist
| Lifestyle Factors | Benefits for Breast Health |
|---|---|
| Maintaining a Healthy Weight | Reduces hormone levels that promote breast cancer growth |
| Regular Exercise | Reduces breast cancer risk through improved overall health |
| Limiting Alcohol Consumption | Reduces the risk of breast cancer associated with alcohol consumption |
| Breastfeeding | Offers potential protection against breast cancer |
| Regular Check-ups and Screenings | Facilitates early detection and timely treatment |
Conclusion
Early detection is crucial in the successful treatment and management of breast cancer. By being aware of how to check for breast cancer through self-exams, screenings, and recognizing symptoms, you can take control of your breast health and increase the chances of early detection.
Regular self-exams allow you to become familiar with the normal look and feel of your breasts, making it easier to identify any changes or abnormalities. Complementing self-exams with clinical breast exams and mammograms as part of routine screenings can further enhance early detection efforts.
It is important to remember that early detection is not a substitute for professional medical advice. Consulting with healthcare professionals and following their guidance is essential in managing your breast health. They can provide personalized recommendations based on your individual risk factors and help you navigate the process of screenings, biopsies, and genetic testing.
Stay proactive and prioritize your breast health by adopting a healthy lifestyle, maintaining regular check-ups, and following recommended screening guidelines. By taking these steps, you are empowering yourself to play an active role in your breast health and ensuring the best possible outcomes in the fight against breast cancer.